Touching the Untouchable: Reflectionsfrom 153rd Course of Somatosensory Pain Rehabilitation in Montreal - Hande USTA OZDEMIR
USTA OZDEMIR Hande, PhD, PT[1]
Pain is something we encounter daily in our clinical practice and yet, it remains one of the least tangible experiences we try to understand. This paradox drew me to Montreal, where I attended the four-day Somatosensory Pain Rehabilitation course, a program that explores the intricate relationship between sensation, the nervous system, and pain perception (Finnerup et al., 2016).
Learning Through Real Experience
The course stood out for its step-by-step, hands-on teaching. The concept flowed naturally into practice, bridging theory and clinical application in a way that made neuroscience tangible. Rather than abstract lectures, we learned through real patient cases, real materials, and real-time evaluation and treatment demonstrations. This experiential learning brought depth to the neuropathic pain.
Two core clinical examination signs aesthesiography & allodynography guided this somatosensory investigation (Fig. 1):
Figure 1: A moment from our lesson with Eva LÉTOURNEAU about somatosensensory testing.
Aesthesiography allowed us to map the patient’s pain and sensory territories according to cutaneous nerve branches, revealing where normal and abnormal perception met.
Allodynography focused specifically on areas of pain provoked by normally non-painful stimuli, helping to visualize the extent and intensity of allodynia on the skin’s surface.
Both tools made neuropathic pain visible transforming a subjective symptom into a tangible, mappable experience (Spicher, 2006; Packham et al., 2020a).
Using monofilaments calibrated in grams, we applied graded pressures to define sensory thresholds and document changes across sessions. We also used two-point discrimination testing to assess the quality of hypoesthesia and cortical representation. Variations in discrimination thresholds reflected how the brain’s sensory maps had been distorted by persistent pain and how these could normalize through somatosensory rehabilitation (Spicher, 2006).
Another innovative assessment we practiced was the Rainbow Pain Scale, a colour-coded visual system used to document pain intensity and quality across mapped zones. Unlike numeric rating scales, it provided an intuitive, spatial picture of pain, allowing both therapists and patients to track sensory recovery over time. Seeing colours shift as sensitivity improved was both clinically informative and emotionally empowering for patients (Packham et al., 2020b).
Ee also used the McGill Pain Questionnaire (MPQ) to complement these spatial and perceptual tools, and to capture the qualitative and quantitative dimensions of pain, including sensory, affective, and evaluative descriptors. The MPQ allowed us to document the patient’s pain experience in words, giving insight into the emotional and cognitive aspects of chronic pain a reminder that sensation and perception are inseparable from meaning and experience (Melzack, 1975).
Rethinking Our Role: “Avoid as Much as Possible to Touch”
One phrase from instructors stayed with me: “Avoid as much as possible to touch.” At first, it seemed counterintuitive after all, our professions are grounded in the therapeutic use of touch. But the meaning became clear as the course progressed. When the nervous system is sensitized, even gentle contact can reinforce protective responses (Finnerup et al., 2016). Our task, then, is not to fix through touch, but to guide through perception.
This concept reshaped how I approach patients with allodynia or hypoesthesia. Instead of rushing to desensitize or mobilize, the process begins with understanding and respecting the nervous system’s protective behaviour. Only once allodynia is resolved can we gradually address hypoesthesia a multistage rehabilitation process that honours the body’s readiness to re-engage with sensation (Spicher, 2006).
The Science Behind the Practice
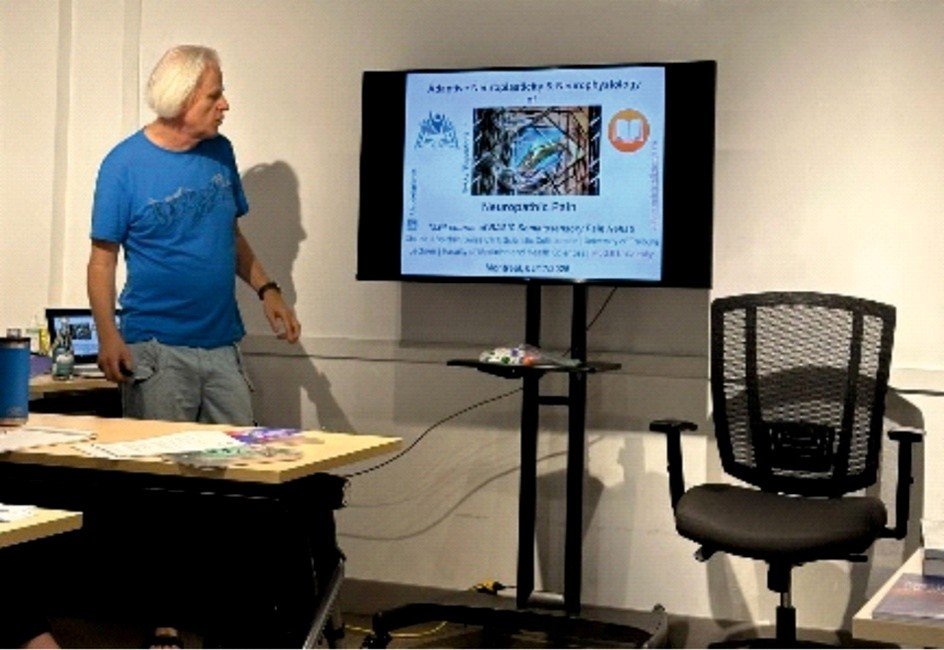
Figure 2: Claude J. SPICHER explaining the principles of adaptive neuroplasticity in somatosensory pain rehabilitation.
What made the Somatosensory Pain Rehabilitation course particularly valuable was its balance between neuroscience-based techniques and practice-based evidence. We explored how pain is not a direct reflection of tissue injury but rather a multifactorial experience produced by the brain. Altered cortical maps, disrupted sensory integration, and maladaptive plastic changes all contribute to persistent pain (Flor, 2003; Butler & Moseley, 2013; Finnerup et al., 2016).
Through the method of Somatosensory Pain Rehabilitation (SPR) we can help the brain reinterpret somatosensory input, through adaptative neuroplasticity mechanism (Fig. 2) as safe again. It’s a process of re-educating the somatosensory nervous system, retraining discrimination before desensitization (Spicher, 2006).
This approach also reminded me of the importance of neuroanatomy not as static knowledge, but as dynamic territory. To treat effectively, one must “learn all the domains of the nerves along the body.” Each cutaneous branch, each peripheral pathway, can tell a story about the patient’s pain. Understanding these pathways allows us to connect symptoms to structure and perception to physiology (Spicher et al., 2020).
Comprehensive Learning Resources
Another strength of the course was its educational design. We received well-curated and meticulously written books and booklets that covered both theoretical and clinical aspects of the method of SPR (Spicher, 2006; Spicher et al., 2020). These materials provided detailed illustrations of nerve domains, testing protocols, and rehabilitation stages, making it easier to review and retain the knowledge long after the course ended.
For me, these resources served as a bridge between learning and clinical integration tools I now reference when planning somatosensory rehabilitation programs or when teaching colleagues/students about somatosensory rehabilitation.
Collaboration and Case-Based Learning
A defining feature of the course was the collaborative narration. Instructors and therapists discussed cases openly, building a shared understanding of each patient’s somatosensory profile. The discussions highlighted how neuropathic pain is rarely simple. This team-based reflection mirrored what real rehabilitation should be a partnership between clinicians and patients. Beneath the surface symptoms lie layers of neural adaptation, fear, and misunderstanding. Addressing these requires not only manual skill, but curiosity, patience, and the willingness to see each case as an evolving narrative (Butler & Moseley, 2013; Finnerup et al., 2016).
From Course to Clinic
Returning to my own practice, I found myself paying closer attention to the sensory stories my patients tell not only through words, but through the way they move, guard, or react to touch. I began integrating pain questioning, monofilament mapping, and two-point discrimination into my assessments.
The course taught me that these small differences matter. They are windows into the patient’s nervous system and they guide us toward more precise, respectful interventions. It also reminded me that rehabilitation is not about “doing more,” but often about “doing less, with greater intention.”
Conclusion: Re-educating Ourselves About Pain
The Somatosensory Pain Rehabilitation course was more than professional development; it was a professional awakening. It invited me to slow down, observe, and appreciate the complexity of neuropathic pain as a sensory experience.
For physiotherapists and occupational therapists, the message is clear: we must refine our sensory literacy. By understanding how touch, perception, and neural networks interact, we can better guide patients toward recovery not by overriding pain, but by helping them relearn safety through sensation.
In an age when pain science is evolving rapidly, courses like this remind us that progress begins not just in the lab, but in the subtle, everyday moments of clinical practice in the space between hand and skin, where perception and healing meet.
Special Thanks
I would like to extend my heartfelt gratitude to Claude J. Spicher, whose expertise, guidance, and passion for somatosensory pain rehabilitation made this course an exceptional learning experience. His insights and supports were invaluable in shaping my understanding of somatosensory assessment and rehabilitation and continues to inspire my clinical and academic practice.
References
Butler, D.S., & Moseley, G.L. (2013). Explain Pain (2nd ed.). Adelaide, Australia: Noigroup Publications.
Finnerup, N. B., Haroutounian, S., Kamerman, P., Baron, R., Bennett, D.L.H., Bouhassira, D., Cruccu, G., Freeman, R., Hansson, P., Nurmikko, T., Raja, S.N., Rice, A.S.C., Serra, J., Smith, B.H., Treede, R.D., & Jensen, T.S. (2016). Neuropathic pain: an updated grading system for research and clinical practice. Pain, 157(8), 1599–1606.
Flor, H. (2003). Cortical reorganization and chronic pain: Implications for rehabilitation. J Rehabil Med, 35(8), 66–72.
Melzack, R. (1975). The McGill Pain Questionnaire: Major properties and scoring methods. Pain, 1(3), 277–299.
Packham, T.L., Spicher, C.J., MacDermid, J.C., & Buckley, N.D. (2020a). Allodynography: reliability of a new procedure for objective clinical examination of static mechanical allodynia. Pain Med, 21(1), 101-108.
Packham, T.L., Spicher, C.J., MacDermid, J.C., Quintal, I., & Buckley, N. (2020b). Evaluating a sensitive issue: reliability of a clinical evaluation for allodynia severity. Somatosen Mot Res, 37(1), 22–27.
Spicher, C.J. (2006). Handbook for Somatosensory Rehabilitation. Montpellier, Paris: Sauramps Médical [The English translation of Spicher, C. (2003). Manuel de rééducation sensitive du corps humain. Genève, Paris: Médecine & Hygiène].
See also:
Spicher, C., Murray, E., Chapdelaine, S. & de Andrade Melo Knaut, S. (2025). Méthode de rééducation sensitive de la douleur : un nouveau mode de penser la complexité bio-psycho-sociale – Préface : Pierre Sprumont. Montpellier, Paris : Sauramps Médical, 396 pages.
Spicher, C.J., Packham, T.L., Buchet, N., Quintal, I., & Sprumont, P. (2020). (1st English edition stemming from the previous 3rd French edition) – Foreword: B. Kramer. Berlin, London, Shanghai, Tokyo, New-York City: Springer-Nature, 107 pages.
[1] Assistant Professor, Pamukkale University, Faculty of Physiotherapy and Rehabilitation. Denizli TURKEY